Cytokine Release Syndrome (CRS) + COVID
UK ICNARC study (27 March) of COVID and critical care (The ICNARC report contains data on all confirmed COVID-19 cases reported to ICNARC up to midnight on 26 March 2020 from critical care units participating in the Case Mix Programme).
A smart correspondant to Tyler Cowen writes:
“I’ve now seen multiple studies suggesting that up to 80 or 90 percent of patients who end up on ventilators ultimately die. At this point, I guess there’s no way to know if the other 10 percent would have lived without the ventilators. From what I can tell, most other hospitalized patients are getting supplemental oxygen, IV fluids and antibiotics. I have not seen any evidence on the effectiveness of these treatments. Many of those patients live, but we don’t know whether they would have recovered without hospitalization. It would obviously be impossible to do a RCT on that at the moment… “
My reading of those studies is that the death rate - on average - is lower than that - not typically as high as 90% - (the one below is 66%) if you look at the spread of studies. Still, the thrust of the argument is taken.
I have two observations around:
Cytokine Release Syndrome (CRS) + COVID
UK ICNARC study (27 March) of COVID and critical care.
On,
1. A significant number (although exact % seems to be varying) are dying due to the “cytokine storm” or cytokine release syndrome (CRS) that can happen in late stage COVID infection. CRS is an indirect effect (of the immune system going into inflammatory overdrive) which can be devastating.
The Roche drug, an anti-IL-6, Actmera (or tocilizumab) is know to have an anti-CRS effect. The drug is approved in China and is in trials in US. Roche donated drug to Italy as well. Other anti-CRS drugs are also being tested for COVID-related CRS (eg Incyte’s ruxolitinib)
To the extent that ventilators can keep you alive while treatments come on board for CRS, if you develop it, I would expect that to be a positive outcome of critical care.
You will not survive CRS outside of hospital.
As yet, not everyone is using tocilizumab as it’s not approved although mostly the doctor community is aware (I sesne as it’s used against CRS in other areas (for instance, CRS is a major side effect of certain CAR-T cell therapies and anti-IL-6 is used in that setting).
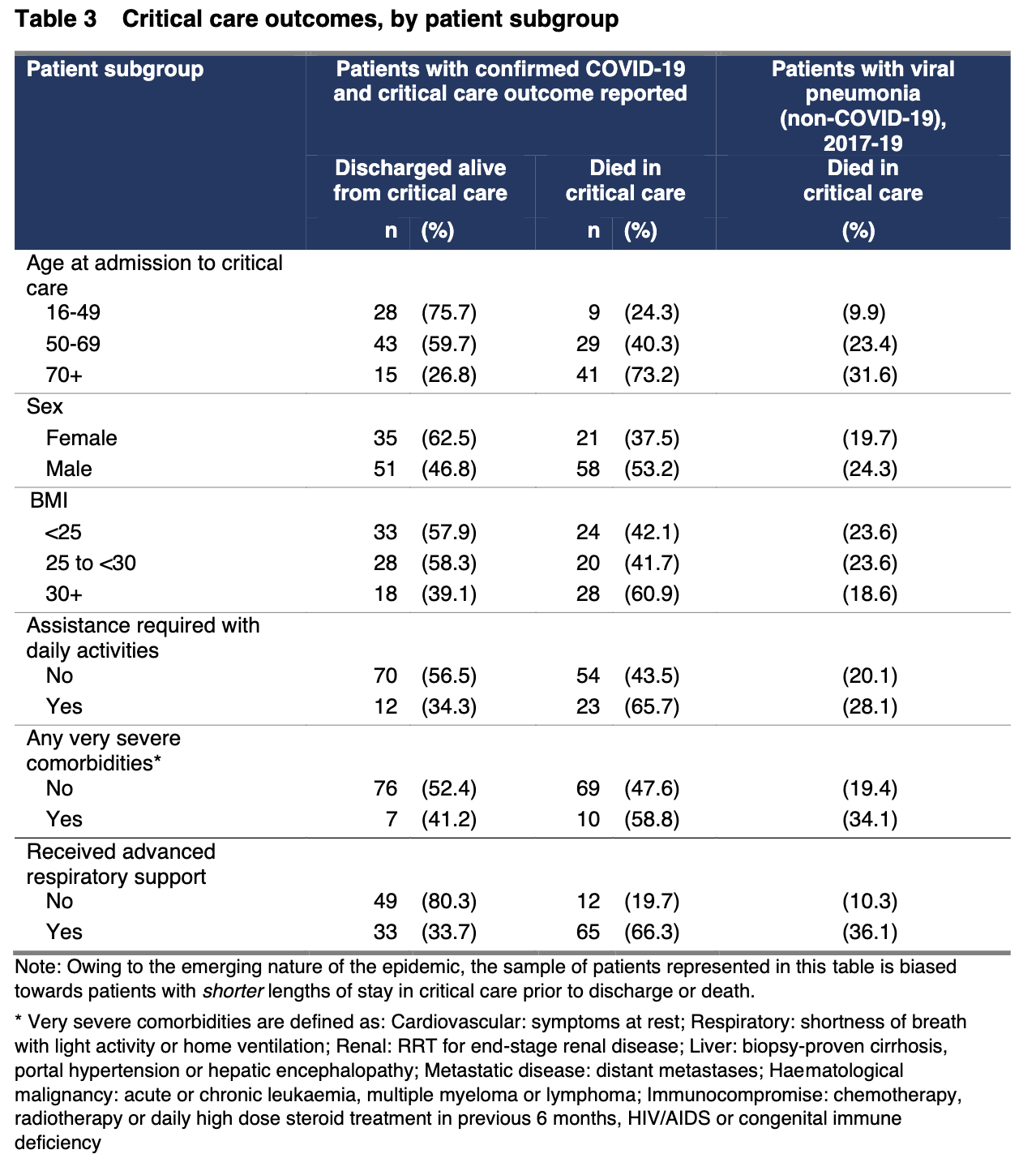
2. There is a small study out of the UK that has compared COVID critical care outcomes to viral pneumonia outcomes. This is not a RCT but it gives some speculative insight:
COVID is hitting males harder (this seems to be now seen in multiple studies). 71% (COVID) vs 54% (viral pneumonia)
Mechanical ventilation: 79% of COVID vs 43% (viral pneumonia, VP)
Survival: 52% (COVID) vs 78% (VP)
Of those who received advance respiratory support 34% survived still low (but not as low as the 80 - 90% figure).
In sum, to me that suggests while hospitalisation is not as life saving as it is with viral pneumonia, there is a benefit to lives saved. One other trade-off is the risk to healthcare workers - especially if the theories around viral load (that doctors are receiving large doses of virus and this is causing more severe disease) are true.
Addendum: FT article looking at Venice vs Lombardy and suggesting hospitals in Lombardy a source of infection
Sources:
Tyler Cowen’s Marginal Revolution Blog: https://marginalrevolution.com/marginalrevolution/2020/04/how-many-lives-is-hospitalization-saving-in-the-pandemic.html
ICNARC study: https://www.icnarc.org/DataServices/Attachments/Download/b5f59585-5870-ea11-9124-00505601089b
Paper on COVID and CRS, Cytokine Release Syndrome: https://www.sciencedirect.com/science/article/pii/S0924857920301047
Lancet article on CRS and COVID: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30628-0/fulltext